Approach to steatotic liver disease in the office: Diagnosis, management, and proposed nomenclature
Canadian Family Physician
APRIL 14, 2025
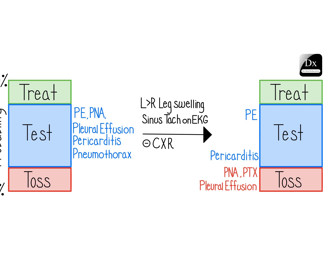
Known complications of metabolic syndrome and advanced liver disease are often present at the time of diagnosis. Subtle differences are present among patients diagnosed with SLD. Courses of action should include assessment of cardiometabolic risk factors and progressive liver dysfunction.












Let's personalize your content