Is there enough time for prevention in primary care?
Common Sense Family Doctor
FEBRUARY 28, 2025
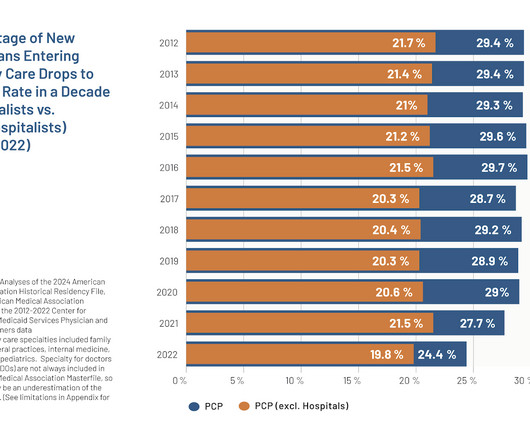
Family physicians are being squeezed by two accelerating trends: (1) too few of us to care for the growing US population and (2) the rising number of tasks that we are asked to accomplish for each patient. hours per day, with more than one-half of that time (14.1 hours) allocated to preventive care.












Let's personalize your content